The study reveals potential options to overcome cancer drug resistance.

When it comes to trastuzumab-resistant HER2-positive breast cancer, a new study conducted at the Johannes Kepler University Linz in partnership with South Korean universities and the Samsung Medical Center is showing very promising treatment options.
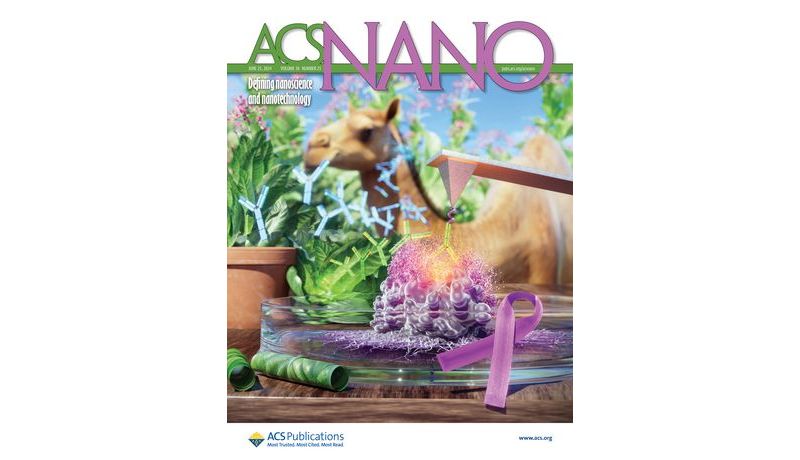
The study is now featured as a cover article in the renowned international journal ACS Nano. A team at the JKU Institute of Biophysics (Doz. Dr. Yoojin Oh), the Department of Mechanical Engineering at Sungkyunkwan University (Prof. Sungsu Park), and the College of Medicine at Chung-Ang University (Prof. Kisung Ko) published a paper on advancements and progress in treating HER2-positive breast cancer.
Leading Form of Cancer in Women
Women's breast cancer is the most common form of cancer in women and each year, the numbers rise. HER2-positive breast cancer in particular is high-risk and constitutes approximately 20% of all breast cancer cases. Compared to other types of breast cancer, this form has a higher recurrence and metastasis rate, meaning the recovery rate is lower. Treating HER2-positive breast cancer often involves trastuzumab, an antibody-based cancer drug used as a targeted form of treatment. The tumor can, however, become HER2-resistant, posing a major challenge in terms of treatment.
Previous studies to date have looked more at the macro level and the way tumor cells interact with the treatment antibodies, paying less attention to the subtle interactions between resistant cells and antibodies.
Observing the single-molecular level
To address the issue, the researchers applied atomic force microscopy-based single-molecule force spectroscopy, allowing them to study the problem at the single-molecule level. To overcome the size limitation and efficiently penetrate tumor tissue, researchers engineered a new type of plant-based and humanized nanobody antibody therapy combining beneficial properties from both animal camelid antibodies and human antibodies.
Dr. Oh remarked: “We attached these tiny nanobodies to a special tip, binding them repeatedly to the tumor cell. It was a bit like fishing. We could see exactly if, when, and how well the therapeutic antibodies would bind to the tumor cell - or not.”
The study also revealed that the nanobody displayed a higher antitumor activity than trastuzumab in immune-deficient mice.
Dr. Oh is hopeful, adding: “If the patient's tumor becomes resistant to trastuzumab, this nanobody-based treatment could be an option.”
Potential large-scale production
The nanobodies are based on stable and inexpensive transgenic plants and could potentially be produced on a large scale, thereby reducing the cost of cancer drugs.
The study marks an important step forward in overcoming the challenges of trastuzumab resistance in HER2-positive breast cancer. If successfully implemented in clinical practice, this plant-derived antibody could potentially revolutionize the treatment and outcome of patients facing a limited range of available treatment options.
The JKU biophysicist is pleased at the successful research on the interaction between cells and cancer drugs at the single-molecule level, adding: “One of the most challenging aspects of treating breast cancer is overcoming drug resistance. Our work is an important step toward solving the problem.”
Research was funded by the Austrian Science Fund (FWF), the Korean NST, the Korean NRF, the Program for Scientific and Technological Cooperation (WTZ, Austrian Federal Ministry of Education, Science & Research), the Ministry of Science, and ICT of the Republic of Korea.
See: https://pubs.acs.org/doi/10.1021/acsnano.4c00360?ref=pdf, opens an external URL in a new window to learn more.